The emotional impact of urinary tract infections in women: a qualitative analysis - BMC Women's Health - bmcwomenshealth.biomedcentral.com
Inclusion and exclusion of participants
In the US, 631 people expressed interest in the study. Of these, 564 did not meet inclusion criteria, 15 withdrew from the study after being recruited due to personal reasons, and 12 did not attend the scheduled interview. In Germany, 90 people were contacted, of whom 45 did not meet inclusion criteria, five did not want to download an app required for an associated mobile ethnography exercise, and 15 did not meet quota criteria. A total of 65 participants completed the in-depth telephone interview, 61.5% from the US and 38.5% from Germany.
Participant disposition and characteristics
Participant characteristics are summarized in Table 1.
Of the women interviewed, 73.8% were between 18 and 49 years of age. Most participants either had a uUTI at the time of the interview or had experienced one within the past 3 months. Similar proportions of participants had experienced either less than three or three or more uUTIs in the past year. Approximately half of the participants had received one course of antibiotic treatment for each uUTI experienced in the past year.
Domains and major themes in the emotional experience of uUTI
Analysis of the interview texts focused on three domains of participants' statements about their uUTI journey: (1) experience of physical symptoms, diagnosis, and treatment; (2) impact of uUTI on life activities and relationships; and (3) the emotional impact of these experiences (Table 2).
We estimate saturation was achieved after analysis of 20 US participant interviews and 17 German participant interviews. High levels of consistency were observed across the sample, regardless of whether the participant was from the US or Germany, with the exception of the financial impact. Where applicable, differences by country, demography, or clinical profile have been noted in the report of findings. Major themes that emerged from the inductive analyses are summarized in Fig. 1 and described in detail below.
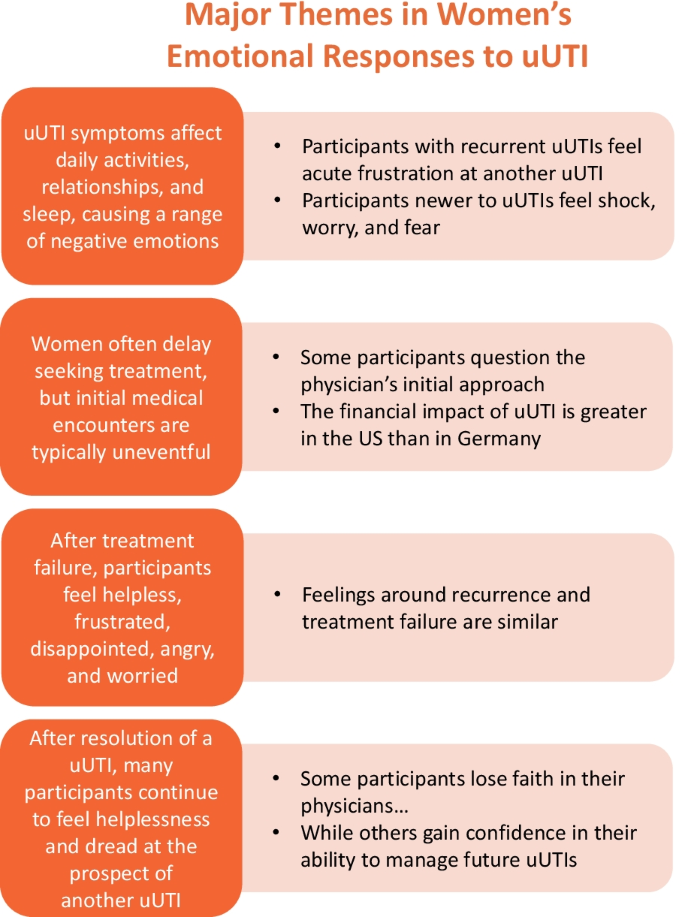
Themes emerging from analysis of interview texts. uUTI uncomplicated urinary tract infection
Wide range of negative emotions due to uUTI symptoms
Interference with life activities
Symptoms of uUTI affected multiple areas of daily life, including activities, relationships, and sleep (Table 2). Participants described missing work, study, family, and social commitments, which caused significant disruption. Bathroom stops interfered with daily routines of work, chores, and childcare. Participants also experienced reduced effectiveness at tasks because of pain. One participant said, "Pain kept me from functioning fully in everyday life" (DE18).
Participants were frustrated by the interference of uUTI symptoms with day-to-day life. The continuing need to be close to a bathroom led to difficulty in keeping up with day-to-day activities and therefore frustration and anxiety, as well as embarrassment (especially if "caught short," as one participant put it). Taking time away from school and work led to high levels of stress and frustration. Impacts on normal routines (e.g., childcare) led to feelings of helplessness due to lack of control.
Regarding experiences at work, participants described frequent toilet visits, vigilance to ensure a bathroom was nearby, and worry about odor associated with the infection. A participant said, "You're thinking, 'What are [my coworkers] thinking? They can totally smell this' … It's kind of like social uncomfortableness … Sometimes I'll go to another floor in the building where I think I won't see anybody I know" (US19).
Difficulty in visiting the doctor for treatment also affected daily life and caused stress and anxiety. Some participants expressed irritation at trying to obtain a doctor's appointment and having to spend time in the waiting room. One participant said, "Going to the doctor makes me very stressed out and irritated, as it is so time consuming" (US14). Many participants expressed a desire for a more efficient treatment process.
Effects on relationships and sleep
uUTIs also caused emotional impacts in the context of relationships. Participants often felt unable and unwilling to involve or share their experience with others, reducing contact and intimacy. The need for frequent bathroom stops when seeing friends resulted in the cancellation of plans, and difficulties in socializing led to withdrawal and loneliness. Participants' low mood also led to negative emotions around interacting with others and again resulted in feelings of isolation. One woman said, "When I have a uUTI it's like I wake up on the wrong side of the bed every day" (US38).
Participants described negative impacts on romantic relationships and intimacy because low mood caused irritation. Abstaining from sex, based on a doctor's advice or symptoms, led to frustration and anxiety. Some participants also mentioned anxiety or the partner mistakenly feeling they are at fault.
Finally, disruption of sleep due to discomfort and getting up during the night resulted in tiredness, irritability, and low motivation, which led to an inability to accomplish day-to-day chores and significant decreases in overall productivity. These impacts on productivity caused feelings of frustration and helplessness. Participants also described irritability due to lack of sleep, which affected relationships with others and led to withdrawal. One participant said, "The sleeplessness is a major problem that affects my ability to function in everyday life" (DE18).
Uncomplicated UTI experienced as an acute, high-impact condition
Participants compared the severity of uUTI symptoms to that of other common, acute, high-impact conditions that are quickly resolved but may recur, such as a cold or toothache. The experience appeared to be low in severity but high in impact. One participant expressed, "It's similar to having flu or a cold—a common illness that many of my friends have had and one that is treatable" (DE25). Another participant stated, "You know when you know you have a toothache coming? I know if I don't do something now about it, in about four to five days it's going to be killing me. That's how I can relate to it sometimes: I know it's coming, and if I don't do something now, I'm going to really regret it" (US22).
Reaction to recurrent and first-time uUTI
Many participants who experienced recurrent uUTIs felt an acute sense of frustration. When symptoms emerged, they quickly recognized they were experiencing a uUTI. These participants were aware of the uUTI process and impact and therefore tended to see the uUTI as an annoyance or frustration. Because of a lack of awareness or expectation of what was happening and what was to come, participants who were newer to uUTIs tended to feel more shock, worry, and fear in response to initial symptoms than participants who had experienced more uUTIs. One participant said, "I woke up because of the pain, and to start with I didn't know what was wrong because I had never had this before" (US40). However, many participants who had not experienced recurring uUTIs still had past experience or an awareness of uUTIs through talking to friends and family to draw on.
Varied experiences with the initial medical encounter
Delays in seeking medical attention
Few participants sought medical attention as soon as symptoms started. Barriers to seeking help included the inconvenience or necessity of taking time off work to see a doctor, wanting to avoid the frustration of a doctor's visit, wanting to solve the problem themselves, hoping the condition would resolve without antibiotics, and reluctance to take antibiotics unless really needed. Some participants in the US referred to cost of care as a barrier to seeking medical attention. One participant said, "I wish I could have a medication on hand, instead of waiting long hours for the doctor" (DE02). A few participants, typically those experiencing their first uUTI, mentioned embarrassment as a barrier to seeking care. Common triggers that ultimately prompted participants to seek help were symptoms that did not go away after a few days, pain that worsened to the point of being unbearable, or actively taking a test strip that came back positive.
Financial impact of uUTIs differs in Germany versus US
Based on participants' accounts, the financial impact of having a uUTI differed for participants in Germany and those in the US. Whilst high levels of consistency were observed between participant responses to the emotional impact of a uUTI, the financial impact upon the participant was the key difference between participants from the US and those from Germany. While out-of-pocket healthcare costs are limited in Germany, multiple participants expressed irritation at having to spend money on a uUTI, particularly when purchasing homeopathic treatments. One participant said, "It is difficult to go the doctor, time-consuming and so on, so sometimes I try to treat it with products that I can buy at a pharmacy, and that can cost quite a lot" (DE19).
For some participants in the US, the financial impact was perceived as irritating. One woman explained, "It's $35–$40 every time you get a uUTI. It's a little ridiculous for something supposedly one in three women experience multiple times a year" (US36). However, for other participants in the US, the financial burden was much greater. Missing work to attend a doctor's appointment was sometimes difficult if the participant did not have sick leave. Out-of-pocket payment for a doctor's visit and treatment, particularly for participants who were uninsured, meant difficulty paying other bills and led to stress and frustration with the financial shortfall. One participant stated, "I end up having to miss out on work [to attend a medical appointment]. Because I am paycheck to paycheck, I fall behind. And it has a snowball effect for me. It's frustrating … Eventually I will catch up on my bills, but I do fall behind" (US21).
Varied emotions and understanding related to uUTI treatment and management approaches
Participants may use their previous experience to guide treatment discussions with their physicians
Participants with an infrequent history of uUTI were often satisfied with the treatment discussions with their physicians, attaching little to no emotion to the conversation or prescription, with one participant reporting that "I just got it and took it as advised" (DE09). However, participants with a more frequent history of uUTIs felt that their previous experiences allowed them to have more involved treatment discussions with their physicians, with prescribing decisions guided by past experience with antibiotics. One participant reported that "I was aware that it may not work due to my past experiences" (US22). Conversely, some participants with frequent uUTI reported that they did not always feel as though they were being listened to regarding previous treatments and a plan in moving forwards to other treatments, with one reporting that they "asked if we could try something different to see if it worked better—as soon as I finish antibiotics it comes back very soon afterwards" (US27).
Some participants question the need for diagnostic tests
Most participants reported that they had a dipstick test for confirmation of a uUTI. The majority of participants took a pragmatic approach to the need for testing, with an understanding that the test would determine their suitability for antibiotics. One participant reported that "this is standard practice every time I go to my GP" (DE06). Some participants who took a self-management approach mentioned doing an 'at-home' test first to confirm infection and the need for treatment. However, some participants with recurrent uUTI questioned the need for diagnostic tests, when they deemed the diagnosis to be obvious.
Participants are frustrated by the burden of time needed for visits to their physicians
In addition to frustration in requiring a positive diagnostic test, some participants reported frustration at the burden of time needed for visits to their PCP. Participants with recurrent uUTI felt they knew when they had another uUTI, and therefore felt they should be prescribed treatment without the need for a visit to their physician: "It is frustrating that you cannot call the doctor and get the prescription based on your reporting of symptoms and knowledge that you have a uUTI" (US36).
Treatment failure causes frustration and anger
Trying to understand treatment failure
Among participants who experienced treatment failure, most reported going back to the same physician or clinic as they did for initial treatment. In explaining treatment failure, some physicians provided a basic explanation of bacterial resistance. Participants were generally relieved to have an explanation for treatment failure and motivated to receive a second antibiotic to resolve symptoms. One participant said, "Bacteria are too stubborn. I didn't really ask for much detail, I just took [the antibiotic] because I wanted the UTI to go away as quickly as possible" (DE01). When the physician offered no explanation for the treatment failure, participants sometimes felt responsible and blamed themselves. In the words of one woman, "I was asking myself whether I did something wrong: sitting on a cold surface, not drinking enough…" (DE03).
Emotional reactions to treatment failure
Participants who experienced treatment failure described many feelings, including helplessness that the antibiotic was not working, frustration at "going round in circles," disappointment that treatment did not work, irritability because nothing seemed to be working, anger at having to go to the doctor again (which was seen as inconvenient), exhaustion with continuing symptoms, and worry ("Is something underlying?" "Is this my fault?"). One participant said, "You're irritable. You don't want to be bothered. You're taking pills and nothing seems to be working. And you're not sleeping … Sometimes I just feel like I'm going around, and around and around and around" (US22). When offered a second antibiotic, participants described feelings of worry and concern about whether the new treatment would work, as well as frustration and annoyance at having to take another round of antibiotics. A participant said, "I cried in the practice, because I was frustrated and in despair" (DE02).
Similarity of feelings about recurrence and treatment failure
There was substantial overlap in the emotional experience of uUTI recurrence and treatment failure of an acute episode. With both recurrence and treatment failure, participants experienced the same feelings of continual suffering, as well as the same experience of having to continually revisit the doctor. Participants described feelings of frustration at suffering from yet another uUTI impacting their life and routine; helplessness because of a "hamster wheel" effect of continually suffering and visiting the doctor; dread and anxiety because of the expectation of another uUTI, as well as anticipation of the negative symptoms to come; and worry that there was an underlying issue causing treatment failure or recurrence (Fig. 1).
Prospect of recurrent uUTIs provokes dread and helplessness
Fear of the next uUTI
After resolution of a uUTI episode, participants continued to experience residual feelings.
Anticipation of the next uUTI and the pain and disruption it would bring caused dread and a feeling of helplessness in participants with frequent uUTI. Indeed, one woman described this feeling as, "Here we go again" (US42). Participants who suffered very frequent uUTIs expressed helplessness that the problem kept returning and anxiety at the prospect of another infection being just around the corner. Participants became anxious about suspected triggers of uUTIs, such as a new sexual partner, restarting birth control pills, giving birth, stressful life experiences, and even cool weather. Some participants described feeling helpless that they are in a permanent cycle, waiting for the next uUTI. A participant said, "I felt trapped. Like I couldn't break free or away from it. I was trapped in a cycle of having these UTIs back to back and I couldn't seem to break free" (US32).
Loss of trust in physicians
Participants who experienced recurrent uUTIs sometimes raised concerns with the physician, and they expressed a lack of trust in their HCP if requests were not responded to. Women experienced anxiety and anger that treatment was not working or that further problems were not investigated. One participant said, "I asked if we could try something different to see if it would work better. In the past, as soon as I finished the antibiotics, the problem came back very soon afterwards" (US27). Some participants described not feeling they were "heard" regarding previous treatments and their desires for the management plan moving forward, which led to frustration with and distrust in their HCP. Belief in the physician was questioned, and some participants considered changing PCPs or visiting a specialist. One woman said, "I do not have high expectations from medical professionals—doctors have missed things before" (US19).
For some, new feelings of resourcefulness
In contrast, a few participants described positive developments after having experienced recurrent uUTIs. Some received specialist referrals after repeated treatment failure or recurrence, and these participants expressed relief at undergoing further investigations. A few participants suffering from recurrent uUTIs mentioned feelings of positivity when they found ways of keeping the problem controlled. A participant said, "I did recover faster because I was drinking more water, so now I feel like I've got a little more empowerment every day to prevent them" (US46).
Comments
Post a Comment